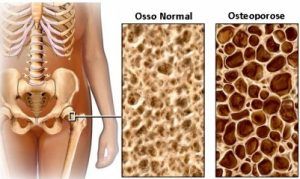
Osteoporosis, also called osteoporosis, is a condition in which the bone contains more and more openings: it becomes more porous. This is because more bone is broken down than new bone is made, i.e. the balance between bone production (osteoblasts) and bone breakdown (osteoclasts) is disturbed. Osteoporosis symptoms are the disappearance of calcium and other minerals from the bone and the weakening of the bone structure. This also shows that ‘bone decalcification’ is actually not a good term, because more minerals than just calcium (calcium) play a role. Because the condition often only gives rise to symptoms at a late stage, osteoporosis often only comes to light as soon as the elderly suffer a bone fracture. The bone tissue is then weakened to such an extent that a bone fracture or collapse of the vertebrae can already occur with a small load. Osteoporosis leads to an increased risk of bone fractures, especially of the spine, hip, wrist, upper arm and pelvis.
There are roughly three types of osteoporosis (bone loss):
Type 1. This concerns women after the menopause (menopause). This is where the drop in estrogen levels plays an important role. Osteoporosis is more common in women than in men.
Type 2. This is a progressive osteoporosis. It affects men and women. As we age, the body naturally breaks down more bone than it makes.
Type 3. Secondary osteoporosis. This is due to other health problems. Conditions such as diabetes, rheumatism, thyroid abnormalities or bone marrow tumors can lead to osteoporosis. But the use of certain medicines, such as corticosteroids, antidepressants, anticonvulsants, chronic heparin use or antacids can also promote the development of osteoporosis.
Symptoms
Osteoporosis symptoms are often non-existent and in most cases the condition does not cause any symptoms. There is an increased risk of a bone fracture, but these often only occur at a higher age.
Sometimes a vertebra collapses causing the back to curve or a person shortening as they get older.
Causes
Risk factors for developing osteoporosis are:
• Insufficient exercise
• Too little calcium, silicon and other minerals important for bone health in the diet
• A vitamin D deficiency
• Drinking more than 2 glasses of alcohol per day
• Smoking
• Women after the transition (menopause) due to hormonal changes
• Heredity
• A high homocysteine level
In addition, people with underlying conditions such as diabetes, joint problems, COPD and thyroid disorders have a greater risk of osteoporosis. As well as people taking medications including corticosteroids, antacids and antidepressants.
Nutritional advice
• Ensure the intake of sufficient calcium through the diet (min. 1000 mg per day) and, if necessary, supplement deficiencies in vitamins D3 and K2 with a dietary supplement to optimize calcium absorption in the intestines and bones.
• Get calcium mainly from vegetable sources, such as green (leaf) vegetables, nuts, seeds and beans. Full-fat dairy products in moderation.
• Limit the intake of alcohol, caffeine, phytic acid and oxalic acid to improve mineral absorption.
• Consumption of predominantly alkaline foods (PH > 7) can benefit bone health.
• Watch out for an elevated iron status in postmenopausal women. An excess of iron in this group has been linked to the development of osteoporosis.
• Eat a healthy and varied diet with enough vegetables, fruit, fatts and proteins to get as many nutrients as possible for strong bones.
Comments
If osteoporosis is suspected or to monitor the treatment, the doctor will request a bone density measurement (DEXA scan). During this examination, the amount of calcium in the bones and vertebrae is measured using an X-ray machine. The regular osteoporosis treatment consists of the advice to exercise enough, lose weight if you are overweight and possibly use a supplement with calcium and vitamin D to stimulate bone formation. In advanced osteoporosis, osteoporosis medication, such as bisphosphonates, can be used. Bisphosphonates can cause unpleasant side effects including heartburn, irritation or inflammation of the esophagus and diarrhea.
In addition to the calcium balance, the collagen matrix is also essential for strong bones. Therefore, focus not only on calcium, but also on strengthening the collagen fibers through silicon, vitamin C and collagen.